Hip Impingement – Femoroacetabular impingement (FAI)
One of the most common causes of hip pain is hip impingement. Research tells us that 87% of patients presenting with hip pain fit the diagnostic criteria for hip impingement, also known as femoroacetabular impingement or ‘FAI’.
The Anatomy and Function of the Hip Joint
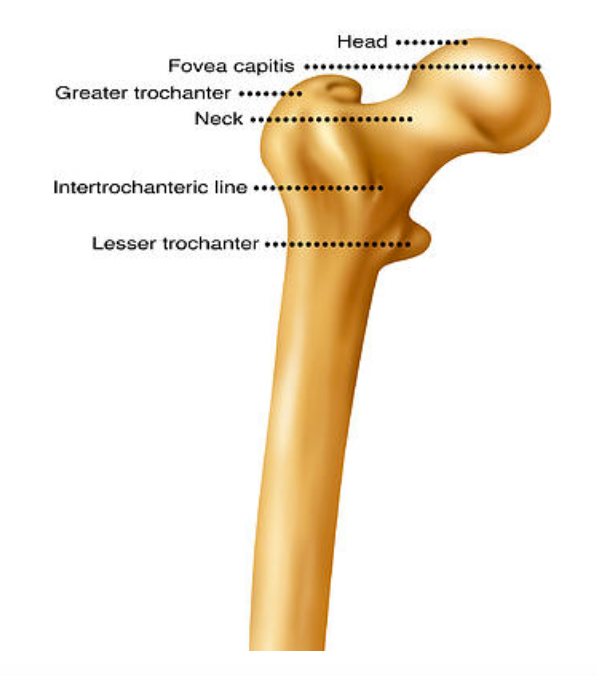
The hip joint is a ball and socket shaped joint. The pelvis houses the circular concave ‘socket’ part of the joint, known as the acetabulum, and the top of the thigh bone creates the circular convex ‘ball’ part of the joint, known as the femoral head. This circular femoral head morphs into a skinny and beautifully concaved femoral neck. In an ideal world these boney ends are perfectly shaped to create a joint that is terrifically stable yet fantastically mobile.
The shape of your hip joint should be such that it allows you to bend your hips deeply into a low squat, extend to create a long and meaningful stride, move side to side, rotate to allow you to step out of your car, or perhaps your hip mobility allows for great multi-directional agility to maneuver and out-run your opponent. Whether you are an elite sports player or an avid gardener, we all need good hip range to function at our best.
What Causes Hip Impingement?
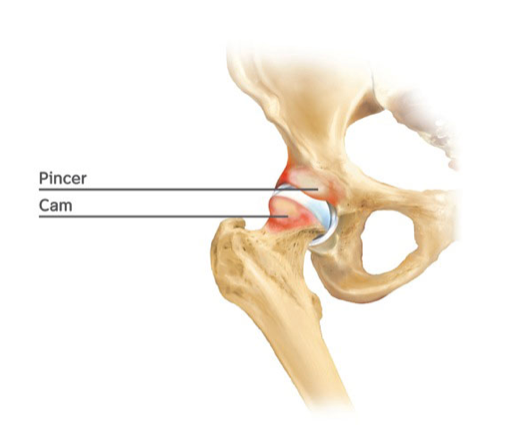
Hip impingement occurs when there is abnormal boney contact between the two parts of the joint, e.g. the acetabulum part of the joint makes contact with the femur when your hip is placed into deep bend. Some examples include a deep squat, sitting in a low chair, cycling, getting out of a car, breaststroke with a frog kick, or moving side to side in a football scrum.
Hip FAI occurs for two main reasons:
1. Changes to the boney anatomy of the hip joint
Research shows that 20% of the general population and 60-90% of the athletic population have variations in the boney shape of their hip joints. These changes can be a deeper hip socket, known as a pincer deformity, and/or a thicker, bumpy femoral neck, known as a Cam deformity. When these boney changes are combined with poor muscular control, this can result in hip impingement, and lead to pain/discomfort.
The athletic population has a high incidence of Cam and Pincer deformities due to the increased load that is placed on the hip throughout development. During an adolescent growth spurt, if a continual load is present, such as a high volume of sporting activity, there will be increased boney lay-down around the hip, resulting in Cam and/or pincer deformity.
2. Dysfunction of the muscles around the hip joint
Despite the presence of a pincer or cam deformity, hip impingement will not occur if the muscles around the hip are functioning well. If the muscles around the hip and pelvis (muscles as high as the core, and as low as the foot and ankle) are firing correctly this will prevent hip impingement. This explains why 50% of the athletic population and 77% of the general population with a Cam or Pincer deformity don’t have hip pain despite the presence of these boney hip changes. So the difference between those that do or don’t have hip pain is THE MUSCLES!
If the muscles around the hip are weak this can result in poor hip control and alignment, with the resultant effect of hip impingement and pain.
Diagnosis
Diagnosis is generally quite simple and in most cases only requires a physiotherapy assessment. During this assessment we perform different hip tests, including one particular hip test called FADIR (anterior impingement test) that is 90% accurate in detecting FAI.
Other important assessments include:
Analyzing your posture, how you move, including how you walk, squat and balance
Hip range of motion
Specific hip tests
Muscle strength assessment
This may include a hip screen assessment using a hand-held dynamometer, which is a small device with a force plate. This device allows us to measure the strength of the different muscles around the hip and pelvis. We can assess for symmetry and balance in the body. We know from research that your right hip muscles should be as strong as your left hip muscles (even if you have a dominant leg), and that certain muscle groups should be stronger than others. For instance, particular gluteal muscles shoulder be stronger than your hip flexor and groin muscles.
Your physiotherapist will be able to guide you on the need for other helpful diagnostic tools such as a plain hip x-ray, or an MRI+contrast.
How Physiotherapy can help
Once a detailed physiotherapy assessment is completed a specific treatment plan can be developed that is centered on your goals and help you return to the activities you love.
This treatment plan can include:
Advice on pain relief
Advice on activity modification
Manual therapy (massage, myofascial release, dry needling, cupping) to reduce muscular tension around the hip, restore range of motion and reduce hip pain
Specifically tailored exercise rehabilitation to address muscle weakness and improve the muscular support to the hip joint. This rehabilitation is not limited to the muscles around the hip but may also involve the core, foot and ankle muscles.
Specific stretching
Physiotherapy management varies greatly between individuals, as no one hip is the same. The period of time to rehabilitate the hip also varies, but it generally takes 2-6 weeks to see an improvement in hip symptoms and 6-12 weeks to improve the strength of the muscles around the hip.
At TPS we work closely with your medical team, such as your GP, orthopaedic surgeon and/or sports physician. If a patient has not had an improvement in their hip pain after 6 weeks of rehabilitation we will refer onto a specialist.
If you or someone you know suffers from hip pain, come and see one of our friendly pelvic physiotherapists for a thorough assessment and treatment plan. Hip pain is 100% treatable, so make a start to a healthier and happier hip!